Understanding Gluten Sensitivity and Coeliac Disease
Mindd Foundation

Gluten Sensitivity is now referred to as the ‘No Man’s Land’ of digestive disorders. Understanding Gluten Sensitivity is firmly placed as one of the most controversial topics in nutrition, and indeed medicine as a whole.
There are likely two reasons behind this controversy:
- Firstly, many will argue that gluten sensitivity is simply a health trend or fad. It’s hard to argue with that; the topic displays all the hallmarks of a nutritional fad including celebrities espousing the benefits of gluten-free living.
- Secondly, the medical profession regards gluten sensitivity as a very grey area when it comes to a clinical diagnosis. If a patient does not have Coeliac Disease (an allergy to gluten) there should be no reason why these patients cannot consume gluten.
So, what evidence exists for gluten sensitivity, and where does pathology testing feature in distinguishing gluten sensitivity from Coeliac Disease?
Understanding Gluten Sensitivity versus Coeliac Disease
It is essential to explain the difference between true Coeliac Disease and other potential issues with gluten. This will give patients a better understanding of symptoms they may be experiencing, when they need to seek medical advice, or when it might simply be safe enough to try eliminating gluten from their diet.
-
Coeliac Disease
People with Coeliac Disease have an allergy to gluten. Gluten is a protein that is found in the grains wheat, barley, rye and oats. Even a few molecules of gluten can cause severe illness in someone with Coeliac Disease. The cardinal signs of Coeliac Disease are diarrhoea, signs of malabsorption (including nutritional anaemia’s such as iron, B12 and folate deficiencies) and weight loss. All foods and beverages made from these grains must be strictly eliminated from the diet and this should be done under medical supervision, not through self-prescription of the diet
-
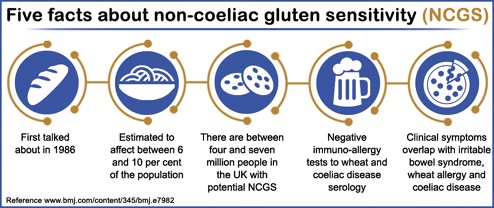
Gluten Sensitivity
This is often referred to by other names such as Non-coeliac Gluten Sensitivity and Gluten Intolerance. Gluten in the diet is speculated to cause a range of adverse effects, including abdominal pain and bloating, lethargy, lack of concentration, excessive wind and fluctuations from abnormal bowel habits including constipation and diarrhoea. Patients with gluten sensitivity do not have an allergy to gluten in the true pathological sense, but they report an improvement in their symptoms if gluten is removed or reduced in their diet.
It is important to remember that many signs and symptoms of gluten sensitivity are the same as other medical conditions (some which can be quite serious, including gynecological and other gastrointestinal conditions). If you are unwell with any of the above issues, it is imperative to have medical assessment to rule out serious medical conditions and establish the possible cause of your ill health
Mechanism of Action
The underlying problems causing both Coeliac Disease and Gluten Sensitivity are different.
In Gluten Sensitivity, no allergic or autoimmune reaction is noted. All pathology tests essentially return normal results. It is usually a diagnosis of exclusion, meaning that all known possible diseases have been tested for thoroughly, and excluded. If the symptoms resolve on a gluten-free diet and return upon a gluten challenge, the diagnosis is cemented even further.
Conversely, Coeliac Disease involves injury to the microstructure of the small intestine, essentially the ‘lining’ of the small intestine (see diagram below). Microscopic, finger-like projections known as villi and microvilli (responsible for nutrient absorption) are destroyed. Under the microscope, a person with active Coeliac Disease will have no visible villi projecting into the lumen (the hollow space) of the small intestinal tract. Also present will be numerous white blood cells and other immune cells characteristic of inflammatory and allergic response.
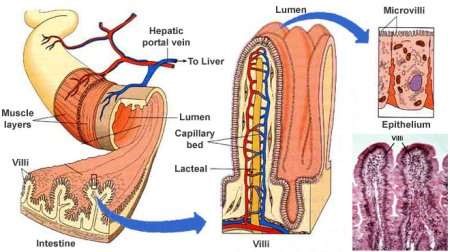
Diagram: Microstructure and histology of the small intestine. Source: Textbook of Medical Physiology, Guyton and Hall.
Understanding Gluten Sensitivity and the Clinical Implications
Some people rightly suspect they have an allergy to gluten and experiment with a gluten-free diet. The problem here is most people adhere to the diet with varying degrees of compliance, thus the testing is never complete or accurate. They return to eating gluten having never consulting a doctor or nutritional professional.
Additionally, eliminating gluten-containing foods does remove large food groups from the diet, and appropriate healthy food replacements should be discussed with a health professional to eliminate the possibility of nutritional deficiencies. This is especially important in children, pregnant women and the elderly.
At present, no blood or other pathology tests definitively establish a diagnosis of gluten sensitivity. It is very possible that gluten sensitivity is transient, with certain, even individually unique factors provoking episodes of digestive illness following gluten ingestion.
Factors that may provoke gluten sensitivity and be self-limiting include:
- gastrointestinal infections
- changes in gluten load
- physiological stresses such as surgery or pregnancy
Some patients test transience by adding gluten to their diet after achieving remission to see if it can be tolerated and if so, how much can be taken with impunity. Establishing a ‘threshold’ of how much gluten can be tolerated is an option for those patients with non-coeliac gluten sensitivity.
Written by Annalies Corse BMedSc, BHSc.
References
- The Gastroenterological Society of Australia (2016). Coeliac Disease. Available at: http://www.gesa.org.au
- Dodou, K and Whitely, P (2014). Non-coeliac gluten sensitivity — a look at the evidence behind the headlines. The Pharmaceutical Journal. Available at: http://www.pharmaceutical-journal.com/news-and-analysis/features/non-coeliac-gluten-sensitivity-a-look-at-the-evidence-behind-the-headlines/11132494.article
- Ferdu, E (2009). Between Celiac Disease and Irritable Bowel Syndrome: The “No Man’s Land” of Gluten Sensitivity. Available at: http://www.nature.com/ajg/journal/v104/n6/abs/ajg2009188a.html
- Holmes, G. (2013). Non coeliac gluten sensitivity. Gastroenterology and Hepatology; From Bed to Bench. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4017515/
- Kagnoff, M. (2007). Celiac disease: pathogenesis of a model immunogenetic disease. JCI Insight. Available at: http://www.jci.org/articles/view/30253